Samuel Gandy became an Alzheimer’s disease researcher in part to help his own family. He watched his mother spiral downward as she lost her memory and then her ability to care for herself.
After that, Gandy, now director of the Center for Cognitive Health at the Icahn School of Medicine at Mount Sinai in New York, thought his research might help prevent a similar fate for himself. Now in his 60s and having watched every single promising drug trial for Alzheimer’s fail, he’s had to give up on that idea, too.
Gandy is now focused on helping the next generation of young scientists who work in his lab and others. “Now I just want to contribute to the eventual eradication,” he says. “As long as I feel like I’m moving the ball down the field in the right direction, that’s worthwhile.”
The repeated failures of Alzheimer’s drugs in late-stage, hugely expensive trials, have forced Gandy and other researchers to recalibrate any optimism about finding a cure. With the annual Alzheimer’s Association International Conference currently finishing up in Los Angeles, scientists are still hopeful about the future—but that future now seems a lot further away.
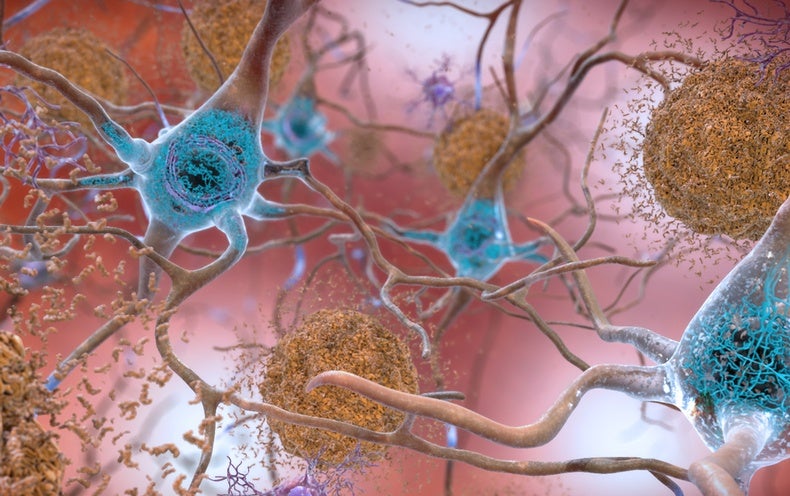
For three decades, most researchers assumed that the cure for Alzheimer’s lay in getting rid of the build-up of a protein called beta-amyloid in the brain. Eliminate that bad actor, and the disease would be vanquished, the thinking went. Then, when that failed, researchers thought they had to get rid of the beta-amyloid earlier—let it spread too far and clog up too much and there was no way the brain could bounce back, researchers assumed.
Yet all the recent trials of early-stage patients proved that idea wrong, too. Amgen, Novartis and the federal government announced at the conference that they were ending their latest anti-amyloid trial, because the drug harmed more patients than it helped. Nearly everyone has now given up on the idea that fighting amyloid will be enough to combat Alzheimer’s on its own once damage has begun.
There are 102 drugs being tested right now in patients, according to the Alzheimer’s Drug Discovery Foundation. Most are in mid-stage trials, meaning they’ve already been shown to be safe in a small group, but have not gone through the rigorous testing in patients to determine whether they are effective. Maybe one will turn out to make a big difference. Yet few researchers believe in the prospect of a magic bullet. Scientists think that it’s more likely that a combination of approaches will be needed to prevent, treat or cure Alzheimer’s, similar to how a drug cocktail is needed to treat HIV.
Two research pursuits seem to hold the most promise—though both might need to be used in combination with each other, perhaps along with anti-amyloid approaches. The first is addressing a protein called tau. Tau causes tangles of material in the brain that clog it up, compounding the problems of beta amyloid. Getting rid of tau is looking more and more promising as part of a cocktail of approaches, says Kenneth Kosik, a professor of neuroscience, and co-director of the Neuroscience Research Institute at the University of California, Santa Barbara.
The second area focuses on inflammation. There’s some indication that an immune reaction—perhaps from something as seemingly benign as the microbes that cause cold sores or gum disease—could be a spark that launches a series of events that ultimately lead to an Alzheimer’s diagnosis.
Researchers are even starting to question the assumption that Alzheimer’s must be treated before the brain has deteriorated. “There’s a lot of biological reasons for why that may not be true,” says Howard Fillit, a neuroscientist, geriatrician and founding executive director and chief science officer of the Alzheimer’s Drug Discovery Foundation.
Cholesterol-lowering statins were developed for people who already had a first heart attack, Fillit notes, and whether they can prevent that first one remains controversial. With Alzheimer’s, he says, it’s a good idea to treat people before symptoms have become disabling, but he’s not convinced it makes sense to treat 55-year-olds who might someday go on to develop the disease. Such research could take decades to prove out, and if a drug can’t reverse or freeze early symptoms, he’s not sure it could prevent them from ever occurring.
In the meantime, a growing consensus has emerged that, although a drug treatment is desperately needed, people can take concrete steps to reduce their risk of developing Alzheimer’s. “Prevention is the key element if we want to manage this epidemic,” says Miia Kivipelto, a professor, senior geriatrician, and director of Research, Development, Education and Innovation at the Karolinska University Hospital in Stockholm.
Fillit, also a clinical professor at the Icahn School of Medicine, notes that lifestyle modifications such as statins and quitting smoking have already reduced dementia rates, which have been falling for the past few decades—though the raw number of patients has grown as more people live long enough to develop the disease. Roughly 5.8 million Americans currently live with dementia, according to the Alzheimer’s Association.
One new study published on July 14 in JAMA looked at nearly 200,000 people from the U.K. and showed that an unhealthy lifestyle can increase someone’s chances of developing dementia. A healthy lifestyle, in contrast, can reduce that likelihood, even among those at high genetic risk, the study found.
Kivipelto leads a series of prevention trials called FINGER, for Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability. The global program started in three countries and has now spread to 25, which will eventually yield more information on the impact of lifestyle on Alzheimer’s risk.
There are six basic things it’s already clear people should do to lower risk, Kivipelto says:
- Exercise regularly—tons of evidence shows that physical activity can significantly reduce the risk of Alzheimer’s, with a new study finding that exercise slows Alzheimer’s even after amyloid has begun to build up. It’s not clear yet what precise amount or intensity of exercise provide the most benefit, but Kivipelto says “you don’t need to get to elite level sport.” She recommends the U.S. federal guidelines of at least 150 minutes of exercise or other movement a week, including both aerobic activity and muscle training.
- Eat a healthy diet, with lots of vegetables, fruits and healthy oils. Some older people will have to work to get adequate nutrition, whereas others will struggle to keep their weight under control.
- Keep your brain active. She and other experts remain skeptical about computer games designed to stave off Alzheimer’s (as they mostly improve people’s skill at playing computer games). But one study published in Neurology just before the conference found that people who participated in more mentally stimulating activities—such as reading, using a computer, participating in social activities, playing games, or craft activities—lowered their risk of mild cognitive impairment, which precedes dementia.
- Reduce risk factors for cardiovascular disease by addressing high blood pressure, cholesterol, diabetes and smoking. “What is good for heart is good for brain,” Kivipelto and others note.
- Sleep—both quality and quantity—is increasingly being shown to be important for Alzheimer’s, she says, though it’s not yet clear whether poor sleep in middle age and beyond is a cause of Alzheimer’s or one of its earliest symptoms.
And none of these measures comes with the lengthy list of side effects that accompany drug company ads. Living a healthy lifestyle reduces the risk of chronic diseases by 60 percent and hospitalizations by 20 percent. “Your health-related quality of life is much better. You feel better,” she says, noting that it’s never too early to start practicing healthy behaviors, but it’s never too late either.
The absence of any meaningful treatments, Kosik says, does not have to be viewed with abject pessimism. “What’s resulted from these amyloid disasters is really 1,000 flowers blooming,” he says. “I think people are exploring a lot of different areas.” Although many venture capitalists are wary of investing in Alzheimer’s drugs after so many failures, Kosik compares investments now to “buying low” in the stock market, when there’s lots of upward potential. “I think we’re in an interesting time right now.”
Although Kosik strongly supports living a healthy lifestyle to reduce Alzheimer’s risk, “we ultimately need drugs,” he says. “We obviously need both…. Lifestyle is no substitute for the drug research that has to be done.”
Funding for Alzheimer’s research has ballooned in recent years, from $400 million in 2013 to roughly $2 billion in 2018, boosting research and adding to the field’s sense of optimism.
That federal bump ends next year, and after that, funding is uncertain. To keep the momentum going, Gandy, of Mt. Sinai, is looking to the successful fight against HIV/AIDS in the 1990s for inspiration. AIDS activist Larry Kramer annoyed a lot of people, Gandy says, but he also got a lot of scientific attention directed at the disease, which rapidly led to the drug cocktail that now can prevent HIV and keep it under control. So far, Alzheimer’s advocates have been much tamer and more polite, he says—they are all either too affected by the disease, or they belong to a generation trained to be more polite and deferential, or they’re too busy taking care of their loved one with Alzheimer’s.
“Older people think you’re supposed to be nice, and that doesn’t always work,” Gandy says. “We need some loud advocates … the squeaky wheel gets the grease.”
https://www.scientificamerican.com/article/alzheimers-meeting-lifestyle-factors-are-best-and-only-bet-now-for-reducing-dementia-risk/
2019-07-18 10:45:12Z
CBMihQFodHRwczovL3d3dy5zY2llbnRpZmljYW1lcmljYW4uY29tL2FydGljbGUvYWx6aGVpbWVycy1tZWV0aW5nLWxpZmVzdHlsZS1mYWN0b3JzLWFyZS1iZXN0LWFuZC1vbmx5LWJldC1ub3ctZm9yLXJlZHVjaW5nLWRlbWVudGlhLXJpc2sv0gEA
Bagikan Berita Ini














0 Response to "Alzheimer's Meeting: Lifestyle Factors Are Best--and Only--Bet Now for Reducing Dementia Risk - Scientific American"
Post a Comment